
COVID: report of a severe case with a 35-BMI doctor
On admission, O2 supplementation with a mask and venous hydration were started, a chest tomography revealed a ground-glass infiltrate above 50%
10/08/2020
Upon admission, the patient was alert and oriented, 38ºC fever, tachydyspneic, RR 30, tachycardic, BP 120×80, hydrated, acyanotic, O2 saturation was 89%
A 54-year-old male patient was admitted to the hospital with a history of irregular fever for six days, headache, myalgia, cough and dyspnea on exertion. He works as a doctor and has a body mass index of 35. As a comorbidity, he has systemic arterial hypertension and a depressive condition. He is under regular use of alcohol and antidepressant medications.
In the city where he lives and works, an important outbreak of Sars-cov-2 is currently happening. The hospital admission date was June 26, 2020 and in the ICU on June 27, 2020.
Upon admission, the patient was alert and oriented, 38ºC fever, tachydyspneic, RR 30, tachycardic, BP 120×80, hydrated, acyanotic, O2 saturation was 89% Examination of the respiratory system revealed many widespread murmurs and crepitations, the cardiovascular system did not reveal murmurs and abdomen was normal. A nasal swab was positive for Sars-CoV-2.
Upon admission, the use of O2 under face mask and venous hydration were initiated, a chest tomography revealed a ground-glass infiltrate above 50%, as shows figure 01. Intense infiltration in bilateral ground glass was observed. The infiltrate can also be seen in figure 02.
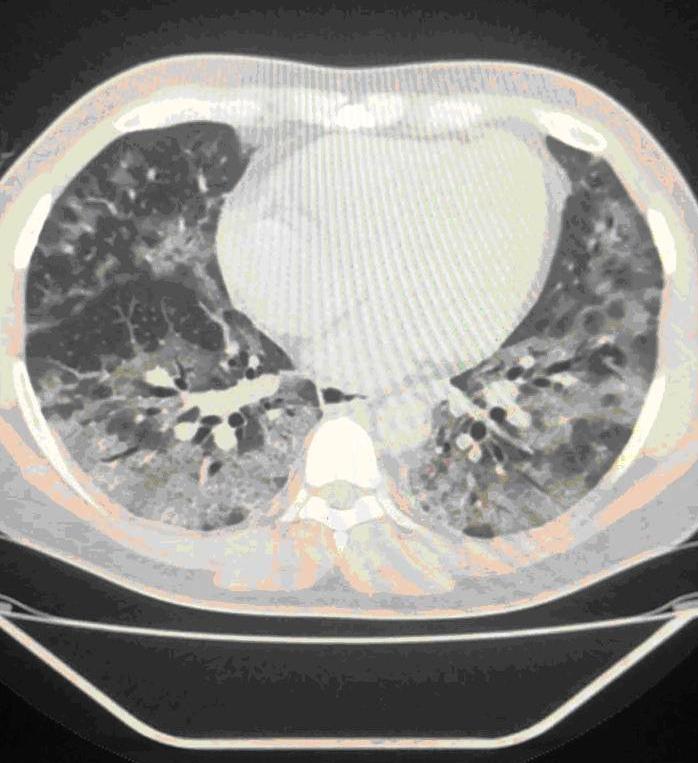
Figure 01: Multiple ground-glass opacities, with a perilobular predominance.
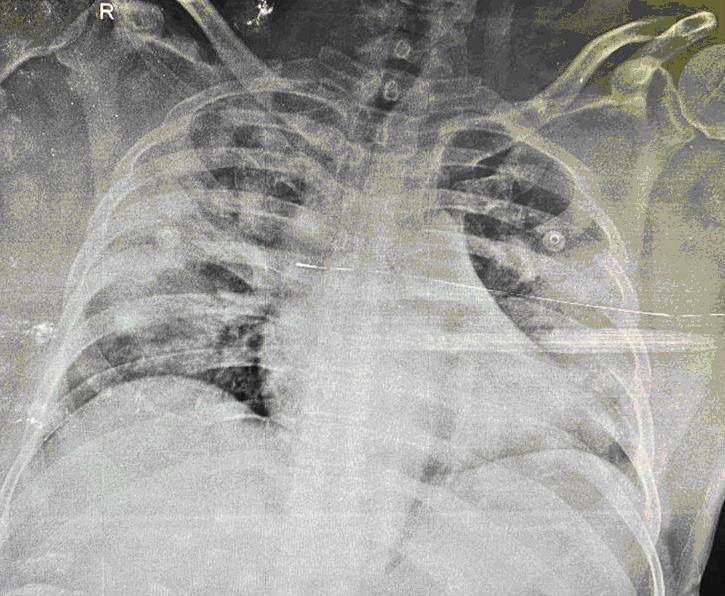
Figure 02 – intense infiltrate verified in the chest X-ray in bed.
The admission blood count revealed HT 45%, 10.000 leukocytes with 7% lymphocytes and platelets of 120.000; 2,0 mg% creatinine, 1200; D-dimer; ALT 60UI / L, AST 70UI / L; 80mg C-reactive protein.
In the following days after admission, there was a significant worsening of respiratory and hemodynamic function. Vasoactive drugs were administered and the patient underwent invasive ventilation. There was a progressive deterioration of renal function and hemodialysis started. Antibiotic regimen with piperacillin-tazobactam started, with posterior substitution by meropenem and linezolid. He did not use corticosteroids, immunomodulators or convalescent plasma. During the most severe period, he was kept under sedation and measures of change in decubitus were optimized, such as pronation to improve gas exchange.
Two weeks after mechanical ventilation, the process of weaning from ventilation, withdrawal of vasoactive drugs started and the patient had progressive improvement. A control nasal swab for discharge from the Intensive Care Unit was negative for Sars-cov-2 on the 21st day after admission.
Currently, the patient is well, vigilant, still undergoing hemodialysis with a discharge schedule for the ward.
The current chest X-ray is seen in figure 03.
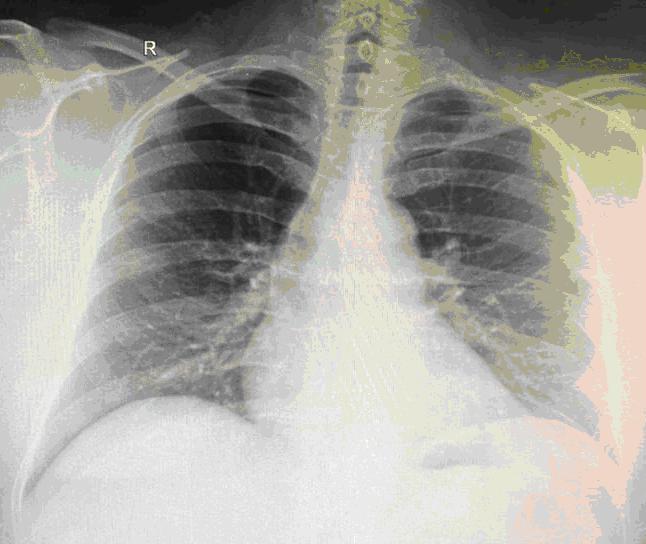
Figure 03 – significant improvement in pulmonary infiltrates.
Brief discussion of the case:
It is a confirmed severe case of Covid-19 that presented respiratory and renal complications. Management was performed only with corrective measures for oxygenation disorders, acid-base and hemodynamics. Antibiotic therapy and physiotherapy were also used as the pronation.
Possibly the use of drugs that interfere with the immune system, such as high doses of corticosteroids, recombinant monoclonal antibodies, convalescent plasma, ivermectin, hydrochloroquine or chloroquine, can negatively impact the patients immune system and worsen the prognosis.
In addition to the recommendation of the dose of 6mg dexamethasone daily or the use of Rendezivir, there is still no recommendation in the literature to use other medications.
We reinforce the need for intensive care treatment in the therapeutic success of these cases.
Collaborated in the elaboration of this case:
Kleber Luz – CRM 2602 – Infectologist, professor at the Department of Infectology at UFRN.
Daniel Calich Luz – CRM 7636 – radiologist.
João Gabriel Villar Cavalcante – CRM 7363 – general practitioner at Hospital Rio Grande – Natal-RN.
* This case was adapted from a real case for illustration purposes.










