
Alert: Brazil should be alert and monitor neuroinvasive arboviruses
Attention to neuroinvasive diseases due to arboviruses must be doubled. Dengue can compromise the nervous system by direct invasion, hypoxia, ischemia, hemorrhage and autoimmunity
09/05/2020
The impact of cases of neurological impairment on the health of individuals and on the installed capacity for assistance in the public hospital network are worrisome factors
Arbovirus infections can result in a wide spectrum of clinical syndromes, from mild febrile illness to hemorrhagic fevers and neuroinvasive forms. In 2015, Brazil saw an explosion in the number of cases of Guillain-Barré syndrome and microcephaly. Under cumulative evidence that infections by arboviruses circulating in the country would be related to the occurrence of congenital and acquired neurological syndromes, in 2017 the Ministry of Health (MoH) launched the “Sentinel Surveillance Manual for Arbovirus Neuroinvasive Diseases”. The document recommended routine investigation for dengue, Zika and chikungunya of neurological cases assisted in sentinel units distributed in each unit of the federation. Currently, the strategy of surveillance of neuroinvasive diseases caused by arboviruses is being reformulated by the Ministry of Health, aiming to simplify the notification instrument and to decentralize and expand research.
For the doctor of virology and coordinator of the surveillance of diseases with neurological manifestations at the Municipal Health Foundation of Teresina and the State Secretariat of Health of Piauí, Dr. Marcelo Adriano Vieira there are few situations as dramatic as witnessing a perfectly healthy adult or child undergoing sudden changes in their personality and behavior, becoming aggressive, delusional, confused, falling into a coma or even dying within a few days after the appearance of mild symptoms (malaise, adynamia, hyporexia, myalgia and fever). “Even when the best treatment efforts are offered and survival is achieved without apparent physical sequelae, families often realize that patients who are victims of encephalitis are no longer the same when they return home, because they have a different personality, irritability, and memory difficulties or motor incoordination”, adds the neurologist.
The 10th epidemiological bulletin from the Ministry of Health on monitoring cases of urban arboviruses transmitted by Aedes indicates that, in 2020, the incidence of dengue cases returns to the endemic channel, with an upward trend in the incidence curve. Therefore, attention to neuroinvasive diseases due to arboviruses must be increased, since dengue can compromise the nervous system through direct invasion, hypoxia, ischemia, hemorrhage and autoimmunity, says Dr. Marcelo. Still according to him, studies carried out in the state of Piauí indicate that 0.6 to 3 cases of neurological impairment can occur for every 1000 reports of dengue, Zika and/or chikungunya arboviruses. In face of this expectation, the impact of neurological impairment cases on the health of individuals and over the installed capacity for assistance in the public health network are worrying factors.
Estimating the exact incidence of acute viral encephalitis is very difficult, because many cases are diagnosed as meningitis with neurological complications or are considered as metabolic or vascular encephalopathies or as acute psychiatric disorders. “In addition, in most countries the disease is not listed for compulsory report and the identification of the specific virus that causes it is difficult to carry out”, he points out. However, according to him, viral encephalitis occurs often enough that health professionals need to be familiar with its clinical manifestations, diagnostic methods and therapeutic guidelines. Studies carried out in limited populations have shown an annual incidence between 1-13 cases/100.000 inhabitants.
The Centers for Disease Control and Prevention (CDC) defines the main neurological manifestations of arbovirus infection: meningitis (aseptic), encephalitis and acute flaccid paralysis (myelitis or polyradiculoneuritis). However, other clinical syndromes are admitted as possible manifestations. According to the neurologist, who is also a technical consultant for the General Coordination of Arbovirus Surveillance, of the Ministry of Health, the etiology of many cases of encephalitis remains unknown. “The best research protocols manage to identify the etiology in approximately half of the cases, only. The reduced specificity of the clinical presentation of the various causative agents, the low sensitivity of the diagnostic arsenal available for the known causes of the disease, the restricted use of tests for agents considered uncommon and the possibility of infection by infectious agents hitherto unknown make the etiological diagnosis of acute viral encephalitis a challenge”, he acknowledges.
Current guidelines for the management of viral encephalitis cases estimate that attempts at genomic detection by polymerase chain reaction for herpes virus and enterovirus in cerebrospinal fluid are able to identify 90% of cases with detectable etiology. However, this projection probably does not reflect the Brazilian reality, where several neurotropic arboviruses have proven circulation and where the majority of the population is exposed to the mosquitoes Aedes aegypti and Culex sp. Therefore, the line of investigation of presumably infectious or parainfectious neurological syndromes should take into account these factors and the results of the local series.
Acute viral encephalitis surveillance program in PiauiIn 2013, a surveillance program for acute viral encephalitis and other neurological syndromes was launched in Teresina, Piauí. An investigation protocol was instituted, including research for herpes viruses, enteroviruses, arboviruses, respiratory viruses and Campylobacter jejuni, in partnership with the Central Laboratory of Public Health of Piauí (LACEN) and the Evandro Chagas Institute. “In the midst of this program, the first human case of encephalitis by the West Nile virus in Brazil was detected in 2014. From the detection of this case, the program was adapted to have maximum sensitivity for the detection of new cases, based on the premise that the clinical presentation of neuroinvasive disease by the West Nile virus is, in most cases, indistinguishable among the various other arboviruses , as well as that there is extensive overlap between the clinical manifestations of encephalitis caused by arboviruses, herpes viruses, enteroviruses and several other viral agents”, recalls Dr. Vieira. The program predicted that all acute cases of aseptic meningitis, encephalitis, myelitis, encephalomyelitis and polyradiculoneuritis in the state would be reported and investigated in the laboratory.
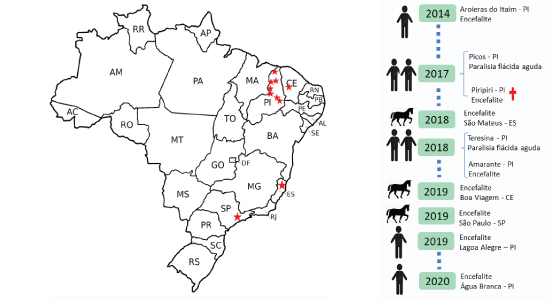
West Nile fever cases in humans and animals in Brazil, including one case with a lethal outcome. Serological tests of 39 other human cases in Piaui tested positive for West Nile virus, but with cross-reactivity with other flaviviruses. Previous serological findings also suggest circulation of the West Nile virus among equidae or birds in the state of the Brazilian Pantanal and Northeast
A cut of one year of activity of the program and already under the recommendations of the Ministry of Health showed that arboviruses can be responsible for approximately one third of the cases of encephalitis, myelitis, encephalomyelitis and polyradiculoneuritis in the state, facing the traditional attribution of viral infections from the central nervous system to herpes viruses and enteroviruses and the bacterium Campylobacter jejuni as a trigger for Guillain-Barré syndrome. “In Piauí, the activities of the surveillance program were developed in a decentralized manner, in conjunction with the surveillance of Nile fever. The offensive potential of arboviruses to the nervous system verified in the study may change paradigms in the face of suspected neurological cases that apparently occurred outside a context of systemic infection characterized by fever, rash, arthralgia and myalgia”, highlights Dr. Vieira.
Before the diagnosis of the first human case of West Nile fever in the country, serological surveys carried out using samples of animals (birds and equidae) in the Pantanal and Northeast Brazil showed the presence of antibodies against West Nile virus. To date, human cases have only been reported in Piauí. Three epizootics by the virus in equidae have been confirmed in the states of Espírito Santo (2018), Ceará (2019) and São Paulo (2019) but, paradoxically, no human case has yet been confirmed in these locations. A technical report from the Piauí State Department of Health on the surveillance of West Nile fever between 2014 and 2018, points out that it was possible to infer the etiology of 49% of the reported cases attributable to infectious, parainfectious or post-infectious central nervous system impairment. The local casuistry surprised when evidencing that arboviruses emerged as the most frequent etiology of viral infections of the central nervous system, surpassing the classic sovereignty of herpes viruses and enteroviruses exposed in international case series, considering the cases with inferred etiology.
According to Dr. Marcelo, the report of fever, arthralgia or rash was associated with the diagnosis of arbovirus infection in patients with neurological impairment. However, the carried out investigation suggests that the absence of these clinical manifestations in the notifications is not an adequate element to dispense with the laboratory investigation for arboviruses, since it was related to the likelihood ratio close to the unit. “Although it is essential to consider the herpetic etiology in the face of any case of encephalitis in humans (due to the therapeutic implications related to the urgency of administering acyclovir), such data indicate the need to consider the possibility of an arbovirus being responsible for the infection of the system nervousness of any patient, even in the absence of obvious epidemiological conditions or systemic clinical manifestations indicative of arbovirus”, concludes the neurologist.…










