
COVID-19: cases of mucormycosis grow in India
Mucormycosis is an extremely aggressive disease, which requires diagnosis as early as possible, as well as requires efficacy in therapy
07/06/2021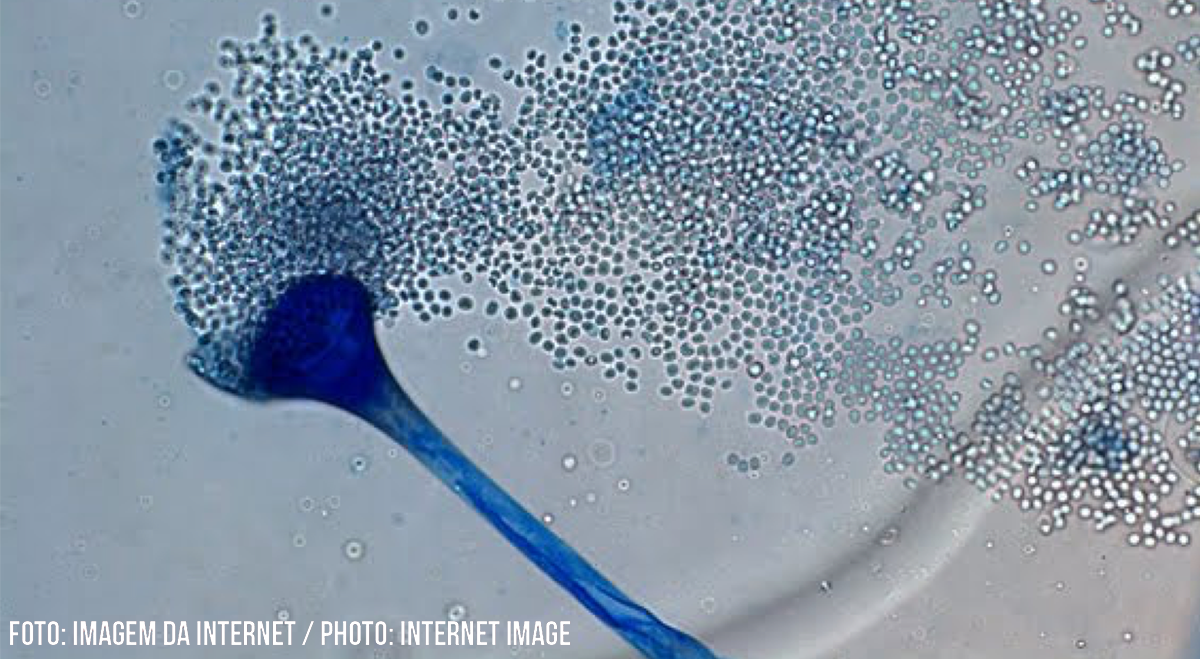
The disease was identified in India even before the pandemic, but cases are growing rapidly in recovered or recovering patients by COVID-19
It all starts with headaches and redness in the eyes. Quickly, a black spot spreads over the cornea. In a few days, the scourge can take over the entire face. These are symptoms of a fungus responsible for a disease called mucormycosis, whose cases in patients recovered or recovering by COVID-19 are growing in India. Mucorales fungi, causative agents of the pathology, are extremely common, being found in the air, the soil, polluted water or in spoiled foods, such as in bread mold. Mucormycosis affects the sinuses, skin, brain and lungs. Often fatal, the disease spreads through the body, destroying skin, muscles, bones and organs. Doctors report that they were forced to remove eyes and bones from peoples jaws in an attempt to prevent the fungus from spreading before it reached the brain, leaving the patient permanently disfigured. The disease was identified in India even before the pandemic, but cases are growing rapidly. According to local information, infections are four or five times more numerous than those detected before the pandemic. Mucormycosis has an overall mortality rate of 50%.
To learn more about the subject, the Communication Office of the Brazilian Society of Tropical Medicine (SBMT) interviewed Dr. Flavio de Queiroz Telles, Infectologist and Associate Professor at the Department of Public Health at the Federal University of Paraná (UFPR).
Check the interview in full:
SBMT: Could you tell us a little about mucormycosis?
Dr. Flavio Queiroz-Telles: Mucormycosis or zygomycosis is considered the most devastating of invasive mycoses. It is a real medical emergency, since Mucormycosis agents grow very quickly both in culture media and in the vascular system of affected patients. It is an angio-invasive disease, initially described by Ptaulf, in Germany, in 1885.
The main risk factors include uncontrolled diabetes, patients with prolonged neutropenia solid organ transplant patients or in prolonged use of corticosteroids.
SBMT: Cases of invasive fungal infection in patients recovered or recovering from COVID-19 are growing in India. What is the reason for this?
Dr. Flavio Queiroz-Telles: India is one of the countries with the highest prevalence of Diabetes Melitus. India is currently one of the countries with the highest incidence of COVID-19. India HAS MANY HOSPITALS AND ITUs in precarious conditions, in relation to sanitary hygienic measures. There are many diabetics with COVID hospitalized in India, most of them receiving, among other drugs, corticosteroids to control lung inflammation by COVID. So, India had an increase in cases of mucormycosis, unlike other countries.
SBMT: Mucormycosis is an extremely aggressive disease, which requires diagnosis as early as possible, as well as effective treatment. In recent months, India has seen thousands of cases. Doctors report that they were forced to remove eyes and bones from peoples jaws in an attempt to prevent the fungus from spreading before it reached the brain, leaving the patient permanently disfigured. Given the similarities between India and Brazil, is there a possibility that the disease will affect patients here? Why?
Dr. Flavio Queiroz-Telles: Mucormycosis is treated with antifungal drugs (Lipidic formulations of Amphotericin B and/or isavuconazole), besides debridement of necrotic tissues, due to angio invasion. Many times structures of the skull and face are removed to save patients lives. So this treatment is normal during mucormycosis. What is worrying is the increase in cases of mucormycosis in India due to the conditions I have already mentioned above.
The incidence of mucormycosis in Brazil has always been lower than in countries in the northern hemisphere, and also than in India. I do not see the possibility of mucormycosis significantly increasing its incidence in Brazil due to COVID. The main invasive angio fungus in Brazil, in onco-hematological patients and also, in patients hospitalized with COVID-19, in ICUs, is Aspergillus spp.
Candida sepsis (Candidemia) is also more important than mucormycosis in patients with COVID, in Brazil
SBMT: Mucormycosis in COVID-19 in Brazil?
Dr. Flavio Queiroz-Telles: It must not be epidemiologically relevant.
SBMT: Are health professionals prepared to diagnose mucormycosis?
Dr. Flavio Queiroz-Telles: Yes, every patient with necrotic ulcerative lesions on the skin, mucosa or with invasive rhinosinusitis, or with pulmonary tomography images with the “inverted halo sign” and negative Galactomannan test, should constitute a diagnostic alert for mucormycosis, especially those with risk factors: uncontrolled diabetics, prolonged neutropenics, and high-dose steroid receptors.
SBMT: Do you understand that it should be treated as an epidemiological emergency?
Dr. Flavio Queiroz-Telles: No, but it has always been an infectious emergency. Nothing should change now in Brazil.
SBMT: What are the differences between mucormycosis associated with COVID19 and Influenza?
Dr. Flavio Queiroz-Telles: The main fungal disease related to Influenza or COVID, in Brazil and in the Northern hemisphere, is invasive pulmonary aspergillosis. Mucormycosis is not frequent among COVID or severe Influenza in Brazil.
Patients with COVID-19, receive high doses of corticosteroids per protocol and stay in the ICU for longer. Influenza can be treated with ozeltamivir, COVID-19 cannot, since we still do not have an effective antiviral treatment.
SBMT: Another infection that has had a greater incidence in the pandemic is candidemia. What explains this increase?
Dr. Flavio Queiroz-Telles: Invasive aspergillosis has been reported more than candidemia
Candidemia in patients with COVID, also occurs due to the risk factors associated with candidemia: prolonged ICU stay, broad-spectrum antibiotics (used in COVID), corticosteroids, central venous catheter, mechanical ventilation, etc.
SBMT: What other invasive fungal diseases are being associated with COVID-19?
Dr. Flavio Queiroz-Telles: There are several, but they are not epidemiologically important.
We have had a case of cryptococcosis, associated to COVID in Curitiba, for example. I am not aware of endemic mycoses, such as sporotrichosis, paracoccidioidomycosis or histoplasmosis associated to COVID.
SBMT: Can mucormycosis affect anyone, of any age? How can we prevent?
Dr. Flavio Queiroz-Telles: Mucormycosis can occur at any age. I am accompanying a 1 year-old child, a bone marrow transplant recipient who survived cerebral, pulmonary and hepatic mucormycosis.
There is no way to prevent mucormycosis, except to control diabetes, and to make an early diagnosis of patients at risk, such as transplanted solid organs and bone marrow, patients undergoing chemotherapy and users of corticosteroids.
High-risk oncohematological patients should remain in wards equipped with a HEPA filter, which retain small particles present in the air, such as fungal spores or conidiums.
SBMT: Would you like to add something?
Dr. Flavio Queiroz-Telles: What happens in India is punctual and has not been observed in Europe, nor should it happen in Brazil.










