
COVID-19: Updates in recommendations of WHO for booster dose
In addition to being safe, bivalent vaccines have been shown to be effective in preventing serious illness, hospitalization, and death
10/05/2023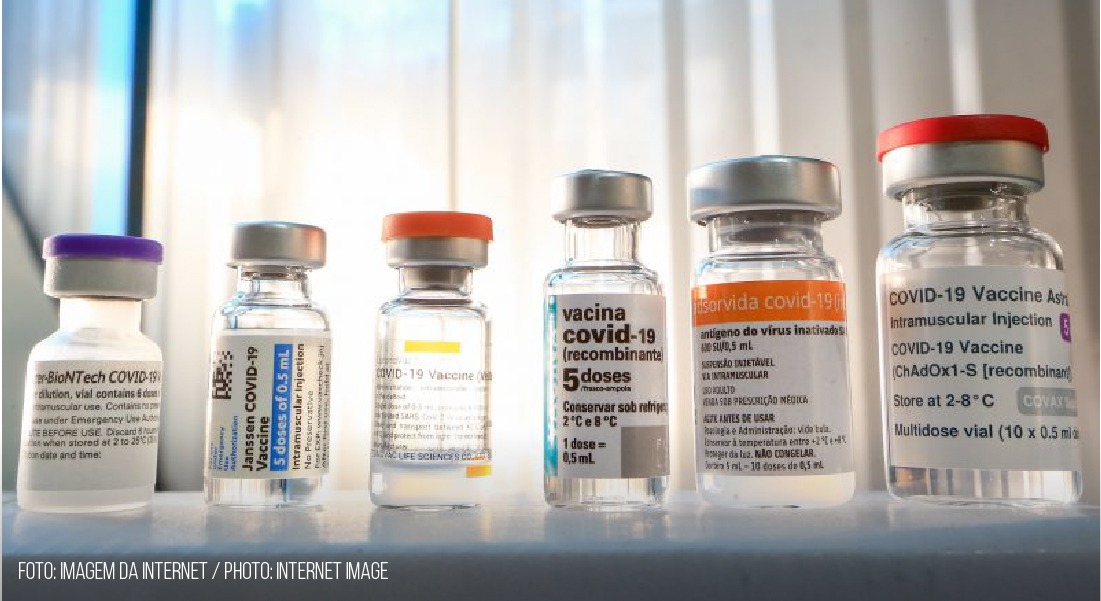
Bivalent vaccines protect against the most predominant variant of COVID-19 , Omicron, and its subvariants
On March 28, the WHO issued a note with updates on recommendations for booster doses of the vaccine against COVID-19. The new guidelines were designed after a meeting held by the Strategic Advisory Group of Experts on Immunization (SAGE) committee in the WHO, which divides the population into three levels of priority according to health risks: high, medium, and low.
Dr. Marta Heloísa Lopes, professor at the Faculty of Medicine of the University of São Paulo (FMUSP), first clarified the misunderstanding regarding the updated recommendations conflicting with those previously published by the WHO. She supported her belief by stating, “It’s not that. In the course of a pandemic, dynamic changes and new measures must be adopted to better face it.” Regarding the new recommendations, Dr. Lopes, who is also responsible for the Reference Centers for Special Immunobiologicals at the Hospital das Clínicas of FMUSP, detailed that the WHO guidelines regarding COVID-19 vaccination prioritized the immunization of the most vulnerable people, namely those with a higher risk of contracting the disease, those that had been severely affected, and those who were dying.
A recent update had revealed that the high-risk groups were older adults and younger adults with significant comorbidities, such as diabetes and heart disease; immunocompromised people, such as people living with HIV; and transplant recipients, including children aged 6 months and older, pregnant women, and frontline healthcare workers. Immunization should be performed within 6 and 12 months after a person’s latest vaccination.
The medium-risk group included healthy adults (generally younger than 50–60 years) without comorbidities and children and adolescents with comorbidities. Dr Lopes recommended the primary series and the first booster doses for the medium-priority group, stating that while other boosters were safe for this group, they had not been routinely recommended, given the comparatively low public health returns.
The low-risk group included healthy children and adolescents aged six months to 17 years. When considering the low burden of disease, SAGE indicated that countries considering vaccinating this age group should base their decisions on factors such as disease burden, cost-effectiveness, and other health programmatic priorities. Dr. Lopes stressed that the primary and booster doses were safe and effective for this audience.
Dr Lopes also pointed out that the WHO had emphasized that these recommendations were short-to medium-term solutions. She stated, “As I have already pointed out, in the course of a pandemic, dynamic changes and new measures may become necessary.” The WHO recommended that countries should make decisions regarding booster doses of COVID-19 vaccines based on the disease burden, the cost-effectiveness of the intervention, and other health programmatic priorities. The organization’s aim was to prioritize vaccinating those who faced the greatest threat of severe illness and death, given the high level of immunity in most of the population worldwide owing to both widespread infections and vaccinations. Furthermore, SAGE called for urgent efforts to move forward with delayed routine vaccinations during the pandemic and warned of an increase in preventable diseases such as measles.
These recommendations were put forward while countries worldwide were adopting different approaches. Some high-income countries, such as the UK and Canada, already offered high-risk COVID-19 boosters this spring, six months after the last dose. In Brazil, a large proportion of the population, including low-risk groups, had access to a third dose. The booster dose was safe for all age groups.
Updated recommendations on bivalent vaccines
In addition to the vaccine schedule guidelines, SAGE updated its recommendations on bivalent vaccines so that countries could consider using Pfizer’s mRNA immunizer (BA.5) for the primary series. Dr. Lopes highlighted that these were as safe as monovalent vaccines and that their side affects would be less adverse. She stated “In addition to being safe, bivalent vaccines, with material from new variants, have proven to be effective in preventing serious illness, hospitalization, and death.
Robust studies have been conducted to determine the efficacy of these bivalent vaccines. One study involving the participation of more than 250,000 people with COVID-19 in the United States noted that these vaccines had an efficacy of 28% (among those vaccinated two or three months ago) to 56% (among those vaccinated more than eight months ago) against hospitalization for the disease. In another study carried out with older adults that had been vaccinated two months prior, the efficacy was 73%. According to him, many studies published in existing literature and practical observations have strengthened the argument that vaccines are effective in mitigating the severity of COVID-19. Dr Lopes explained, “The protection against new infection conferred by these vaccines, however, decreases over time and is relatively short-lived. Added to this is the emergence of new variants of SARS COV-2, hence the need for booster doses.
Reasons for receiving the bivalent vaccine
Throughout history, with respect to health, humanity has experienced difficulties owing to epidemics and pandemics such as the smallpox epidemic, which killed thousands of people; this disease was eradicated through large-scale immunization. Similarly, vaccines are the best tools for containing the spread of COVID-19, which is the most recent global public health emergency. Recently, the Ministry of Health initiated the “National Movement for Vaccination,” with the objective of increasing the vaccination coverage rate of all immunizations offered by the National Immunization Program (PNI), including the vaccine against COVID-19, and launched a campaign for Pfizer’s bivalent vaccine.
Why should I get vaccinated?
- Ending the pandemic: Realistically, the virus may not ever completely disappear; therefore, a potential temporary solution is controlling its spread through measures like vaccination, which can reduce its occurrence.
- Collective protection: The vaccine protects the health of those who have been immunized and the people around them, especially the most vulnerable or those who have comorbidities such as diabetes and hypertension; vaccination is a collective strategy.
- Vaccines are safe; all the immunizers made available to the population have been tested and approved by the National Health Surveillance Agency (ANVISA). After testing is finished, the pharmaceutical company needs to present documentation referring to the results of the research so that ANVISA technicians can verify the safety, efficacy, and quality of the immunizers; the immunizers are only commercialized after all these steps have been completed.
- The booster dose offers even more protection; even with two doses of the primary vaccine, the booster dose may be necessary, according to the recommended dosage for each age group. Over time, the body loses its immunological memory of the virus. A study carried out by the Oswaldo Cruz Foundation (Fiocruz) with more than 1,500 people revealed that after these people took their second dose, the antibodies in their bodies initially dropped and then increased considerably with the reinforcement from the dose.
- Protection against variants: Bivalent vaccines protect against the parent virus, the omicron variant, and its subvariants.
Dr. Lopes recalled that almost all the groups for which the bivalent vaccine was recommended in Brazil had been defined as high priority (most vulnerable) by the WHO. These people responded less to vaccines and lost their protection against COVID-19 more quickly, owing to factors such as age (older adults) or compromised immunity. Dr. Lopes stated, “Reinforcements for these people are extremely important. By decreasing the disease burden in these populations, more patients with other pathologies can be treated by health services. By vaccinating health professionals, fewer professionals will get sick and have lower absenteeism, which compromises the quality of care.”
Anyone who had not completed the primary vaccination schedule with two doses of the monovalent vaccines made with the original strain of the virus were required to do so before taking the bivalent vaccine. Previous vaccines, although less protective against Omicron, still helped reduce the risk of death and development of serious disease, which was why they continued to be included in the two-dose primary vaccination schedule; they are still available in Basic Health Units (UBSs).
Dr. Lopes highlighted the aspects emphasized by the WHO, citing that the impact of vaccinating healthy children and adolescents on public health was comparatively much smaller than the benefits established by traditional essential vaccines for children, such as rotavirus, measles, pneumococcal conjugate, and COVID-19 vaccines for high- and medium-priority groups. Immunocompromised children with comorbidities, who are at greater risk of severe COVID-19, are included in the high- and medium-priority groups; vaccination is recommended for them.
Another aspect mentioned was that countries needed to assess their situation when deciding whether to continue vaccinating low-risk groups, such as healthy children and adolescents, without compromising the routine vaccination that was important for the health and well-being of this age group.
Furthermore, the burden of severe COVID-19 on infants younger than 6 months remains higher than that on children aged 6–5 years. The vaccination of pregnant women—even with an additional dose after more than 6 months have passed since their last dose—protects both them and their developing fetuses while reducing the likelihood that their babies are hospitalized for COVID-19.
Dr. Lopes concluded, “These important aspects must be discussed to identify the most effective measures in terms of public health. The dissemination of these vaccination strategies must include explanations that justify the measures adopted.”
In September 2022, the WHO declared the end of the pandemic. However, the pandemic is still considered to be ongoing. Organizations should only change the officially recognized status of the disease when most countries have proceeded with vaccination efforts, including administering booster doses, improving reporting on data, and increasing the use and long-term availability of immunizers. To effectively leave behind the pandemic, we need to learn to live with the virus; furthermore, everyone should take the recommended doses of vaccines as soon as they become available.










