
Diarrhea in a patient living with HIV
Intestinal spirochetosis is a rare disease, but it can be diagnosed if the doctor is aware of this diagnosis and warns the pathologist about this possibility
14/04/2022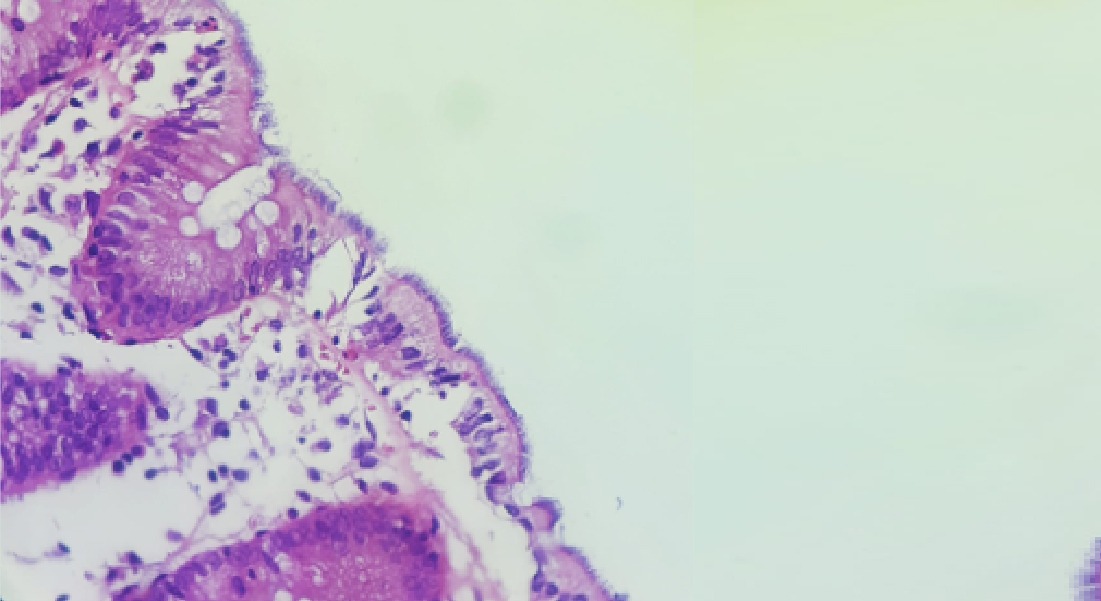
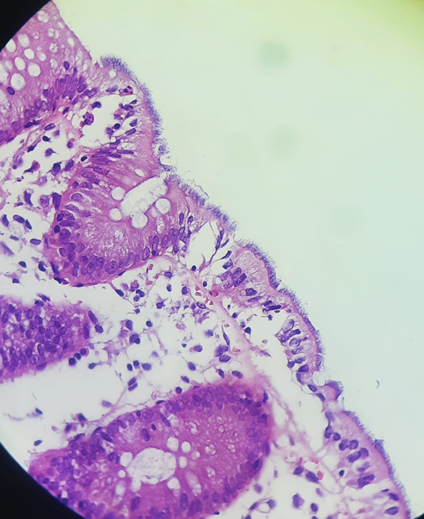
Colon mucosal fragment The large number of spirochetes carpeting the colonic mucosa is observed
Authors:
Lucas Martins Carlos da Silva 1; Vanessa Campos Andrade de Melo Pérsico 2; Jéssica Lajus Fortes Lima 3; Kleber Giovani Luz 4.
Student of the ninth period of the Medicine course at the Federal University of Rio Grande do Norte (UFRN).
Infectologist of the Brazilian Hospital Services Company/UFRN.
Pathologist at the Institute of Anatomopathological Diagnosis MIDAP – Florianópolis – Santa Catarina.
Infectologist, Associate Professor level IV of the Institute of Tropical Medicine of the UFRN.
Case report:
Male patient, 49 years old, born in Natal and coming from Natal – Rio Grande do Norte, bureaucrat, has exclusive sex with men, with a fixed partner for a few years. Lives with HIV, diagnosed in 2015. In use of ART (TDF/3TC + DTG). Never presented opportunistic diseases or required hospitalization for the disease. He has used efavirenz between 2015 and 2016, but changed it to dolutegravir for having presented suicidal thoughts. Last exams: Undetectable Viral Load, CD4+ 594 (Dec/2021). The symptoms began in January 2020.
Main complaint:
Increased frequency of bowel movements and soft stools about 20 days ago
History of Present Illness:
The patient reports that for 20 days he has increased the number of bowel movements to 3 times a day, presenting always pasty stools and abdominal distension at times. Stools with a small amount of fatty appearance and no food debris. Denies presence of: pus, blood, mucus, fever or tenesmus. The condition worsens with the ingestion of milk and alcoholic beverages.
The patient complains that for 15 years, his bowel habit is twice a day, alternating between formed feces and pasty feces. No abdominal distention, pus, blood, tenesmus. On some occasions he made use of antiparasitics with slight improvement, but always returning to the same habit after some time. History of Entamoeba coli and Entamoeba histolytica in a previous protoparasitological, with negative coproculture.
In December/2021 he presented acute rhinosinusitis treated with amoxicillin and clavulonate, with resolution of the respiratory condition.
He does not know whether there was a relationship between the use of medication and the onset of diarrhea.
Morbid history: Systemic arterial hypertension using candesartan, hypertriglyceridemia using fenofibrate 160 mg.
Family history: father and aunt with heart disease. Mother with Parkinsons. Siblings with systemic arterial hypertension and hypercholesterolemia. The Partner also has a diagnosis of HIV infection and is regularly using medication.
Life habits: diet rich in carbohydrates (pizzas, pasta and soda). Cycling and weight training. He drinks 1 glass of wine three times a week and denies smoking. Has 2 healthy dogs and denies contact with sick dogs. Updated vaccination
Bring up the tests from the previous appointment.
Physical examination:
Good general condition, vigilant, conscious and oriented, stained, anicteric, acyanotic, hydrated, without palpable lymph node enlargement, capillary filling time less than 2 seconds.
Vital signs: Heart rate: 84 bpm; Respiratory rate: 14 ipm; Blood pressure: 130×80 mmHg
Oral cavity: well-preserved teeth and absence of plaques or lesions throughout the mouth
Cardiovascular system: Regular cardiac rhythm in two stages, normal sounds, without murmurs.
Respiratory system: present and symmetrical vesicular murmur, without adventitious noises
Abdomen: Discrete abdominal distension, depressible. hydroaerial sounds present, tympanic, free Traube Space, mild pain on palpation and absence of visceromegalies. DB
Lower limbs: no edema and no signs of deep vein thrombosis
Neuro: photoreactive and isochoric pupils. No changes in sensitivity and motor skills
Absence of skin lesions
Complementary examinations:
Undetectable viral load; CD4+ 594; CD8+ 643, CD4/CD8 ratio 0.92 (Dec/2021)
(18/01/2022): Hb 15.1; Ht 45.1%; VCM 91.5; HCM 30.6; leuko 5780; SEG 62%, rods 1%, eosinophils 1%, basophils 0%, lymphocytes 30%, monocytes 5%; platelets 313,000; PCR 6.7 (VR < 10); Total proteins 6.5; albumin 3.9; globulin 2.6; VDRL NR; Hidden blood in feces +; fecal fat. negative; Anti transglutaminase IgA NR; Anti gliadin IgA NR; Anti endomysium NR; Calprotectin 689 (reagent when > 50); lactose tolerance: 96 (fasting), 101 (15 min), 100 (30 min), 99 (60 min) – deficiency when blood glucose rises < 20-25; Cr: 1.2 (TFG: 70); urea 46; GGT 31; TGO 26; TGP 29; Glucose: 95; HbA1c 5.8%; CT: 208; LDL:134.8; HDL: 43; TG: 166; TSH 2.52; TL: 4 D: 1.12;
Colonoscopy: No macroscopic changes. Awaiting biopsy result
Co-culture negative for Salmonella and Shigella and E. invasive coli
Antigen for Clostridium difficile negative (so he did not perform toxins A and B)
Awaiting result of multiplex panels
Serologies: Anti HCV NR; Toxo IgM and IgG negative; CMV IgM – and IgG +; HTLV negative; Chagas and schistosomiasis negative
Ileocolonoscopy biopsy:
Right colon: mucosa exhibits mild mixed inflammatory infiltrate and presence of spirochetes carpeting parts of the epithelial surface, compatible with intestinal spirochetosis. No findings of microscopic colitis
Left colon and rectum: mucosa exhibits mild mixed inflammatory infiltrate and the presence of spirochetes carpeting parts of the epithelial surface, compatible with intestinal spirochetosis. No microscopic colitis findings (Figure 1)
Figure – 01 – Fragment of colonic mucosa. The large number of spirochetes carpeting the colonic mucosa is observed.
Conclusion: Faced with this case, we see the importance of following a step-by-step investigation of diseases and keeping in mind not only the most common diagnoses. Patients living with HIV are more likely to be infected with atypical microorganisms, which we will identify if we follow a logic of investigation based on the syndrome presented by the patient, such as diarrheal syndrome, in this case.
Intestinal spirochetosis is a rare disease, but it can be diagnosed if the attending physician is aware of this diagnosis and warns the pathologist about this possibility. It mainly affects immunocompromised people, especially men who have sex with men. It is possible that in this case a local immunodeficiency, that is, in the mucosa, facilitated the onset of the disease, since the CD4+ count in the peripheral blood was within normal levels, although there was a decrease in the CD4+/CD8+ ratio. In this case, the patient was treated with oral metronidazole with good clinical response.










