
Herpes zoster in a child vaccinated for chickenpox after hand, foot and mouth disease and use of corticosteroids
Although it is more common in older people, herpes zoster occurs with a low incidence in children.
09/02/2022
Vesiculobullous eruption affecting C5 to T2 dermatomes (herpes zoster)
Dorcas Lamounier Costa
Carlos Henrique Nery Costa
Federal University of Piauí
Although vaccine is highly effective against varicella (chickenpox), small children have a slightly increased risk of herpes zoster.This is a 23-month-old child, vaccinated for varicella-zoster (VZV) at 12 months of age, who, after an episode of mouth hand and foot disease (HFMD) developed uncomplicated herpes zoster.
Case Report
This is a 23-month-old boy, weighing 16kg, previously healthy and with normal neuropsychomotor development for his age and with a complete and previously healthy vaccination schedule. On 01/01/2022, he developed a high fever of 39 degrees Celsius, immediately followed by vesicular lesions around the mouth, legs, and arms, without involvement of the oral mucosa, diagnosed as hand, foot and mouth disease. (Figure 1). The symptoms disappeared after four days. A diffuse maculopapular eruption followed, treated with oral corticosteroids. Ten days later, vesicles appeared on the right arm and hand that evolved rapidly and were followed by intense pain and antalgic posture (Figure 2). He was treated with antibiotics and corticosteroids. On the third day, he presented isolated and grouped vesicular lesions, restricted only to the right upper limb. Treatment was started with acyclovir at a dose of 100mg five times daily orally. Laboratory tests to confirm the diagnosis were not made. Two days later, there was a marked regression of the lesions with formation of crusts and the child had no more pain.
Comments
HFMD is quite common and is subject to epidemics and seasonality, transmitted by the fecal-oral route, more common in children under five years of age, in crowded periods, such as on year-end holidays, and as verified in this child. It is mainly caused by a few members of the Picornaviridae, RNA viruses of the genus Enterovirus, particularly coxsackievirus A16 (CVA16) and enterovirus 71 (EV71). The disease often presents with malaise and high fever lasting two days, followed by small vesicles around the mouth, palate and pharynx that can be painful and reduce food intake. The rash occurs on the dorsal surface and palms of the hands and feet, progressing from flat pink patches to elongated gray vesicles, which disappear without scarring. The child did not present lesions in the oral cavity. Occasionally, the illness can become severe.
Herpes zoster is caused by the varicella-zoster virus (VZV). It is an enveloped virus, of the Herpesviridae family, with a DNA genome that encodes about 70 proteins. Infection in humans occurs after exposure of the respiratory or conjunctival mucosa. After primary chickenpox (varicella) infection, the virus migrates along sensory nerve fibers to the satellite cells of the dorsal root ganglia, where it becomes dormant. Reactivation of the virus that has become dormant in the nerve roots leads to shingles. Exactly what causes the virus to reactivate is not known, but emotional stress, medications, exposure to the virus, neoplasms or infections may increase the risk, as happened with this child with HFMD.
Although it is more common in older people, herpes zoster occurs with a low incidence in children, with an incidence of 74/100,000 people-year in some regions of the United States. The incidence rate of children infected with VZV younger than 2 months is significantly higher than of children who had chickenpox between 2 to 11 months of age. The three most curious events in this child were HFMD and the use of corticosteroids preceding the outbreak of herpes zoster and prior and timely vaccination for varicella (chickenpox).
The vesiculobullous eruption is usually restricted to a single dermatome and rarely crosses the midline. It is usually self-limiting and uncomplicated, but postherpetic neuralgia can occur in older people. Occasionally, particularly in immunocompromised patients, it can lead to ocular, neurological, and other complications. In most cases, there is no need for specific treatment, but acyclovir and its prodrugs (such as famciclovir, valaciclovir and penciclovir) can reduce pain and the incidence of post-herpetic neuralgia and are mandatory in cases of complications and in immunosuppressed patients.
The advent of the VZV vaccine in 1995 led to a substantial reduction in the incidence of herpes zoster in children. However, the incidence of herpes zoster is higher among vaccinated children aging two to three years than in unvaccinated children, as is the case with this patient. From the fourth year onwards, there is a clear and significant reduction in the incidence in vaccinated children and, over the years, also in unvaccinated children, due to herd immunity.
The vaccine for VZV is composed of live attenuated virus of the OKA strain. It has 90% protection for chickenpox, 95% for moderate cases and 100% for severe cases. It should be given at 12 and 18 months of age. There are two zoster vaccines available, suitable for people over 50 years old. One of them consists of live attenuated virus (Zostavax®) and the other (ShingrixÒ), approved by Anvisa in the second half of 2021, and made with recombinant proteins and is much more effective.
References:
- Baba K, Yabuuchi H, Takahashi M, Ogra PL. Increased incidence of herpes zoster in normal children infected with varicella zoster virus during infancy: community-based follow-up study. J Pediatr. 1986 Mar;108(3):372-7. doi: 10.1016/s0022-3476(86)80875-7. PMID: 3005536.
- Fong SY, Mori D, Rundi C, Yap JF, Jikal M, Latip ALLBA, Johnny V, Ahmed K. A five-year retrospective study on the epidemiology of hand, foot and mouth disease in Sabah, Malaysia. Sci Rep. 2021 Sep 8;11(1):17814. doi: 10.1038/s41598-021-96083-3. PMID: 34497287; PMCID: PMC8426372.
- Weinmann S, Naleway AL, Koppolu P, Baxter R, Belongia EA, Hambidge SJ, Irving SA, Jackson ML, Klein NP, Lewin B, Liles E, Marin M, Smith N, Weintraub E, Chun C. Incidence of Herpes Zoster Among Children: 2003-2014. 2019 Jul;144(1):e20182917. doi: 10.1542/peds.2018-2917. Epub 2019 Jun 10. PMID: 31182552; PMCID: PMC7748320.
- https://www.gov.br/anvisa/pt-br/assuntos/medicamentos/novos-medicamentos-e-indicacoes/shingrix-novo-registro
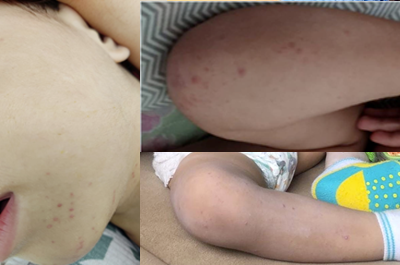
Figure 1. Vesiculobullous lesions affecting the face and distal portions of the upper and lower limbs (mouth, hand and foot disease)

Figure 2 Vesiculobullous eruption affecting C5 to T2 dermatomes (herpes zoster)










