
Integration between national health information systems
Systems integration carried out by the e-SUS AB Strategy can be considered a new fact on the SUS information and IT policy agenda
08/12/2021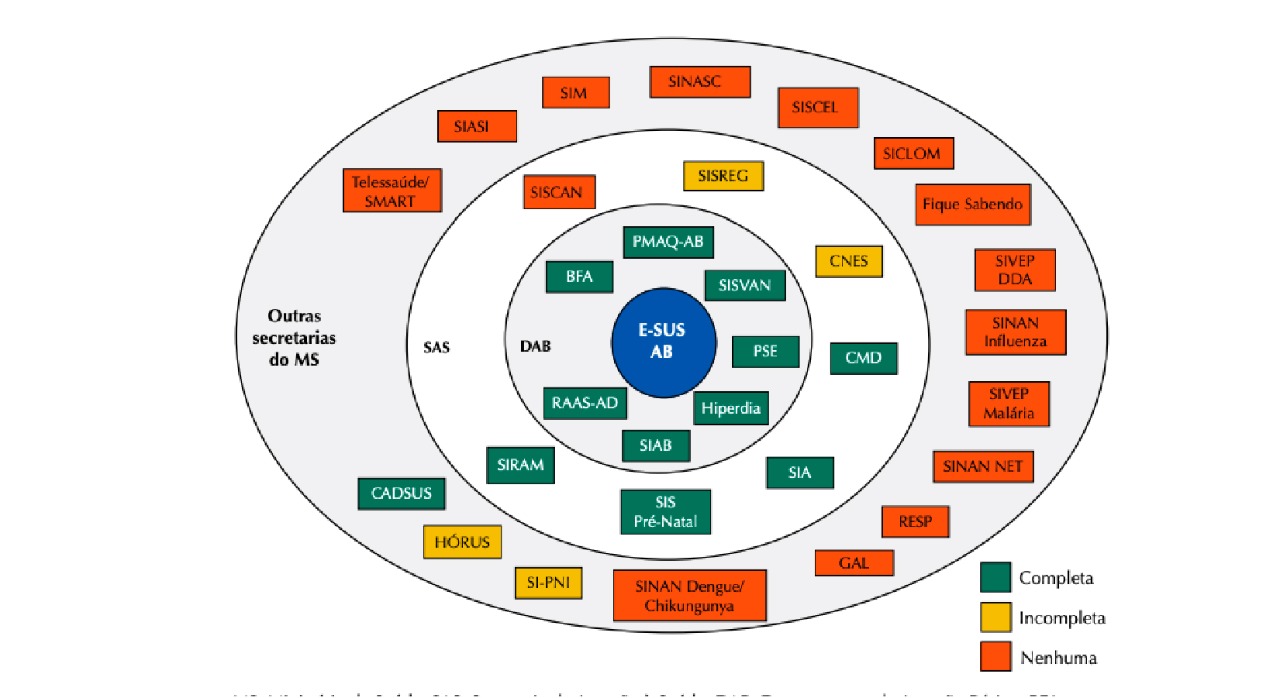
Poor integration means that the same data is filled in different interfaces, generating rework and increased costs, as it becomes necessary to maintain several technological solutions with redundant functions
Within the Ministry of Health, the National Health Information Systems (NHIS) were historically constituted according to specific needs and isolated initiatives from different areas, and not through a broad strategy that considered the health sector as a whole. This caused a deep fragmentation of the information bases of the Unified Health System (SUS), great redundancy in the production of health information in the context of each information system, in addition to forcing health professionals and public managers to coexist with dozens of health information systems at their workplaces. As an attempt to reduce the fragmentation of Health Systems in the SUS, some policies are being implemented, including the e-SUS AB Strategy, led by the Department of Primary Care of the HM.
An article published in November in the Revista de Saúde Pública of the University of São Paulo (RSP_USP) entitled Integration between national health information systems: the case of e-SUS Primary Care measured the degree of integration of the Electronic Citizens Record (PEC) ) of the e-SUS Primary Care Strategy (e-SUS AB) with other NHIS, relating it to the internal political-organizational structure of the Ministry of Health. According to the publication, although still insufficient, the integration of systems carried out by the e-SUS AB Strategy, which focuses on reducing user interfaces, can be considered a new fact on the SUS information and information policy agenda.
The sanitary doctor and Master in Public Health from the São Paulo School of Medicine of the Federal University of São Paulo (Unifesp) and Specialist in Family and Community Medicine from the University of Pernambuco (UPE), Giliate Cardoso Coelho Neto, one of the authors of the article, explains that health professionals are forced to live with many information systems that speak little to each other and this, in addition to causing rework in filling in the information, also harms the patients themselves, who have their data fragmented in different databases. To have an idea, with the pandemic, another information system was created, the e-SUS VE (Epidemiological Surveillance), increasing fragmentation. “With each epidemic, a new system; this has been the focus of health surveillance in Brazil in recent years,” says the author of the study. In his assessment, the fragmentation of systems continues to be a relevant obstacle, even with the progress seen in some areas. He also cites the poor return of information to health professionals and managers as another historical problem, causing them to not have access to the data they themselves produced. Finally, the expert points out an increasingly serious flaw, the confidentiality of personal health data. “The volume of captured data grows exponentially, and the protection mechanisms are still very incipient, giving room for access and misuse of this data,” he warns.
To solve the problem of systems fragmentation in Brazil, Giliate clarifies that an output has been used, the so-called interface integration, that is, when the various data capture interfaces from different systems are unified into just one. Its like an ATM that, despite being connected to several banking systems, has an optimized interface for those who use it, giving the feeling that you are using a single system, he exemplifies by recognizing that the research identified that, when the subject is health information, the historical fragmentation between surveillance and health care remains. “No disease notification system has been integrated into e-SUS. This harms the quality of information and delays the sending of data to the control centers, as health professionals will have to fill in the same data in two or more systems,” points out the researcher. For him, to prevent this from happening, it is necessary to invest in data integration and security, mainly on the part of the federal government, since the large Brazilian health information systems are under its responsibility.
Unfortunately, what has been seen in recent years is the scrapping of Datasus, with frequent episodes of data leakage and the abandonment of solutions that could greatly help health professionals and managers, such as e-SUS Hospitalar (public electronic medical record for use in hospitals)”, he says, who regrets remembering the scrapping of the SUS that has been in rapid progress since the approval of the spending ceiling in 2016. “Just to give you an idea, the SUS federal budget for 2022 predicts a loss of R$ 43 billion, even in the midst of a pandemic. There are no longer financial resources for technological modernization of the SUS, and this lack of funding will cause more frequent episodes of data leakage and delay in the use of digital health solutions, resulting in irreversible damage to the Brazilian population,” warns the researcher who is also a public manager. Finally, Giliate emphasizes that despite the problems, Brazil has a very rich health database built over the last 30 years. “These data were and still have been fundamental in the scientific and technological development of the SUS, in addition to playing a fundamental role in supporting public health policies,” he concludes. The e-SUS AB is the largest electronic medical record in Brazil, provided free of charge by the Ministry of Health to thousands of municipalities.
The investigation
The article was produced from the homonymous masters thesis, defended in 2019 at the Federal University of São Paulo (USP) by Dr. Neto and supervised by Professor Arthur Chioro. The objective was to analyze the integration of e-SUS AB with other NHIS in SUS Primary Care. It is a qualitative case study in which data collection was conducted through document analysis and semi-structured interviews. The first step sought to clarify how many NHIS were in use in SUS Primary Care between 2013 and 2017. Then, to measure the integration, the maintenance of data collection interfaces by the Ministry of Health was applied as a criterion, even after the implementation of the PEC/e-SUS AB.
Between 2013 and 2018, 54 NHIS were identified in operation in Brazil, maintained by the Ministry of Health, including registration systems, notification of diseases and conditions, control and logistics of supplies and medicines, electronic medical records, laboratory management, accounting control of the production of procedures, among others. Systems developed or acquired by states and municipalities were also incorporated into these. During this period, 31 NHIS were found operating in Primary Care, most under the technical management of the Health Care Secretariat (SAS) or the Health Surveillance Secretariat (SVS), 12 of which were fully integrated and in 15 there were no no unification of interfaces with PEC/e-SUS AB. Another 4 have partial integration.
By correlating these data with the political and organizational structure of the Ministry of Health, it showed a greater integration with the systems managed by the Department of Primary Care and a persistence of fragmentation with the NHIS, especially those under the management of the Health Surveillance Department. The disparity between the integration of the PEC/e-SUS AB with the Health Surveillance NHIS is a sign of the persistence of the division and the false dichotomy between Health Care and Health Surveillance practices and processes in the Ministry of Health, even after 30 years of the foundation of the SUS and unification of the state structures of social security hospital care and federal public health in HM.










