
Leishmania: use of centrin-deficient parasites for vaccine development
Currently there are no vaccines available against any of the forms of human leishmaniasis
10/08/2020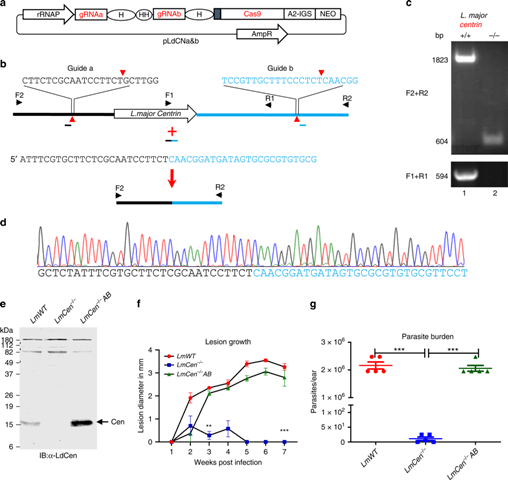
The use of live attenuated parasites, which are not virulent, can also be used to develop vaccines against Leishmania
After most cases of human Leishmania infections, people become resistant to reinfection after clinical cure, suggesting it is possible to develop a vaccines against leishmaniasis. The practice consists on voluntary inoculation, known as leishmanization, that has been used in several countries of the former Soviet Union, Iran and Israel, with live virulent Leishmania parasites, resulted in uncontrolled lesions and has since been abandoned. However, according to a research recently published on Journal Nature entitled “A second generation leishmanization vaccine with a markerless attenuated Leishmania major strain using CRISPR gene editing, this can change. So far, human trials have not taken place, but according to one of the authors, they can begin in a close future.
To learn more about the subject, the Press Advisory of the Brazilian Society of Tropical Medicine (BSTM), interviewed Dr. Hira Nakhasi, Director of the Division of Emerging and Transfusion Transmitted Diseases in the Office of Blood Research and Review (OBRR) at the Center for Biologics Evaluation and Research (CBER) of the U.S. Food and Drug Administration (FDA)
Find the full interview below
BSTM: How you figured out using centrin deficient parasites for vaccination?
Dr. Hira Nakhasi: We started with a foundational insight that some of the most successful viral vaccines are comprised of live attenuated organisms. With respect to human leishmaniasis, although the best protection against reinfection against leishmaniasis has been observed following a deliberate inoculation known as leishmanization or cure from a natural infection, these methods are not safe for the purpose of vaccination. We therefore focused on achieving the safest possible immunization method by creating a genetically modified live attenuatedLeishmania parasite by CRISPR-Cas, the most precise gene manipulation method currently available to us. We targeted the centrin gene for deletion since we showed that deficiency of centrin gene in Leishmania results in amastigote stage specific defects in cell division and yields a mutant parasite strain that is highly attenuated in virulence. We hypothesized that limited replication of centrin deficient mutant Leishmania parasites in the vertebrate host enables the host to develop protective immunity analogous to what has been observed in leishmanization but without any pathology. Thus far all our pre-clinical studies in various animal models confirm that centrin deficient Leishmania parasites could be a potent prophylactic vaccine.
BSTM: How long have been working with these parasites? Can you tell a bit about this very interesting story?
Dr. Hira Nakhasi: Based on the experiences with the successful live attenuated viral vaccines, we thought using live attenuated parasites, that are not virulent, may similarly be used to develop leishmania vaccines. Hence 20 years ago, we started studying the Leishmania biology and identifying genes that may be important for Leishmaniavirulence. Next, we thought if such genes are altered can such parasites be used as live attenuated vaccines. During this process we selected centrin gene which when modified results in Leishmania parasites that has a defect in cell division during the amastigote stage, virulent form of the parasite. We studied centrin gene function and the immunological characterization of the centrin deleted parasites first in Leishmania donovani and more recently in Leishmania major. During these studies, we greatly benefited from our collaborations with experts inLeishmania field in close proximity to us such as Dennis Dwyer, David Sacks, Jesus Valenzuela at the NIH. Key advances in our understanding of protective immunity from centrin deleted parasites as a potential vaccine candidate over the years came from the studies such as the role of polyfunctional T cells, IFN-g+ effector T cells, relevance of testing vaccines against a sand fly mediated infection in various animal models. Our early results with centrin deleted parasites elicited interest in collaborative work internationally including from researchers in Brazil who share the common goal of controlling human leishmaniasis [Ricardo Fujiwara and Rodrigo Oliveira]. More recently, our work with centrin deleted parasites as vaccine candidates advanced further by our collaborating partners from Ohio State University, USA, McGill University in Canada, Nagasaki University in Japan, Pasteur Institute, Tunis and industry partner Gennova Biopharmaceuticals in India. These studies over the years were supported by FDA, NIH, GHIT, Japan and Welcome trust, UK.
BSTM: How successful are similar strategies for other microorganisms such as Mycobacterium tuberculosis?
Dr. Hira Nakhasi: As reported in the literature, similar strategies of vaccination against Mycobacterium tuberculosis and Plasmodium falciparum are in various stages of development and hopefully we should see some promising candidates in the near future.
BSTM: Why do you think there are no available vaccines against any form of human leishmaniasis?
Dr. Hira Nakhasi: In most human infections of Leishmania, people are resistant to reinfection following clinical cure which suggested that it is possible to develop a vaccine against Leishmaniasis. The practice of voluntary inoculation known as leishmanization that was used in some of the former Soviet Union countries, Iran and Israel with live virulent Leishmania parasites from a skin lesion caused by Leishmania parasites often resulted in uncontrolled lesions and has since been abandoned. Safety from unwanted skin lesions was not a guaranteed outcome in this scenario. Vaccine preparations using either killed Leishmania parasites and recombinant antigens or DNA vaccines, approaches that have yielded some highly successful vaccines against viral and bacterial pathogens, have shown to be inadequate in inducing robust protection. As new tools to test the efficacy of anti-leishmanial vaccines became available, we learned that anti-leishmanial vaccines that showed promising results when tested with a needle inoculation in animal model commonly used in the literature, failed to show protection against natural model of challenge i.e., sand fly vector mediated delivery of Leishmania parasites. Suggesting that components from the sand fly vector play an important role in Leishmaniasis, further complicated the development of vaccine. In addition, the complexity of Leishmania genome (~8500 genes, roughly one third of the number of genes in a typical human cell) revealed in the genome studies highlights the potential multivalent interactions between the parasite and its host that result in pathogenesis. Our limited understanding of these problems precluded us from developing an efficacious vaccine.
BSTM: You studied the immunity generated by CD4 T cells and showed that they play a crucial role in the protection against CL. But what about CD8 T cells?
Dr. Hira Nakhasi: Immunization with LmCen-/-parasites induces both CD4 and CD8 T cell responses in pre-clinical animal models. We observed that IFN-g/IL-2/TNFa multifunctional cytokine secreting antigen experienced CD4 and CD8 T cells are induced in the immunized animals. Moreover, LmCen-/-also induce CD8 T cells secreting IFN-g and Granzyme B specific cytotoxic T cell in immunized animals. A definitive role of CD8 T cells in mediating protection needs to be formally demonstrated.
BSTM: Do you think the differential effects of Th1 and Th2 dichotomy in cutaneous leishmaniasis seen in mice is also present in more susceptible species like hamsters, dogs and humans? Do you think the protection conferred by centrin efficient mice will also occur in these species? Why?
Dr. Hira Nakhasi: Yes, we have observed a predominant Th1 type immune response in hamsters, dogs and in human PBMCs similar to mice followingLmCen-/-infection. In addition, we have observed that protection is conferred by LmCen-/-parasites in hamsters against visceral leishmaniasis as well due to the induction of potent protective immunity involving CD4 and CD8 T cell responses.
BSTM: Since centrin is essential in the duplication of centrosomes in eukaryotes including Leishmania why they persist for a while? By the way, how long they persist?
Dr. Hira Nakhasi: We have observed that deletion of centrin allows for a limited replication where amastigotes become multinucleated multi-organelle cells thus affecting their survival in the host. We observed that the centrin deficient parasites fall below the level of detection after 12 weeks. It is possible that a low level of parasites might survive indefinitely as revealed by our immunosuppression experiments.
BSTM: In your paper you stated that L. major remains in the skin at the site of infection and does not cause visceral disease. But how sure are you that they would protect against visceralizing species?
Dr. Hira Nakhasi: From our preliminary studies we learned that LmCen-/-parasites do induce a strong Th1 type of immune response in the lymph nodes as well and immunized animals are protected against challenge with the visceralizing species of Leishmania.
BSTM: Why centrin deficient L. donovani are viable in axenic cultures but not in infected macrophages?
Dr. Hira Nakhasi: Centrin deficient L donovani parasites are viable as axenic promastigotes but are quite rapidly eliminated in axenic amastigote cultures by apoptosis like death indicating that the centrin protein functions in a growth stage specific manner in Leishmania. Centrin deficient L. donovani parasites do not survive in macrophages as you stated since following phagocytosis by macrophages, Leishmania parasites differentiate into amastigotes.
BSTM: Why the presence of antibiotic resistance genes in any attenuated live vaccine renders the vaccine unacceptable by regulatory agencies for human vaccine trials?
Dr. Hira Nakhasi: Regardless of the requirements of the regulatory agencies, it is desirable to have the vaccines preparations free of extraneous materials such as antibiotic resistance genes and other exogenous nucleic acid material, which may otherwise impact vaccine safety and efficacy.
BSTM: Are the results with centrin deficient L. major promising for infection caused by the L. donovani complex or distant related species like Leishmania from the Viannia complex?
Dr. Hira Nakhasi: Yes, in our preliminary studies we observed LmCen-/- immunization protects against L. donovani and it remains to be seen whether similar protection can be obtained against other Leishmania species belonging to Viannia complex.
BSTM: Have you tried to immunize immunodeficient mice with centrin deficient parasites? If not, do you have plans for this?
Dr. Hira Nakhasi: We have tested centrin deficient L. major parasites in RAG, STAT-1 and IFN-g knock out mouse models and showed that no lesions develop in those mice up to 20 weeks after inoculation, which demonstrated the safety characteristics of the mutant parasites. However, we haven’t tested immunogenicity in such mouse models.
BSTM: Have you already started humans studies with centrin deficient L. major?
Dr. Hira Nakhasi: As of now we haven’t started the human studies, however we plan to undertake human studies in the near future with our collaborators.










