
Leishmaniasis: vaccines closer to reality bring hope
Immunizers can have a major impact on improving the quality of life of people living in the poorest regions of the world
10/05/2022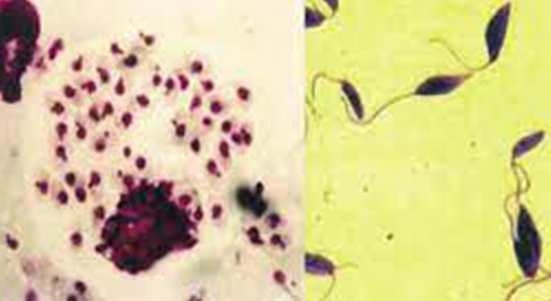
Brazil is the country with the highest number of cases of the three forms of leishmaniasis: cutaneous; mucosal and visceral leishmaniasis, also known as kala-azar
Leishmaniasis, a set of diseases caused by protozoan parasites from more than 20 different species of Leishmania, represents a serious public health problem worldwide. Prevalent in 98 countries, with ~ 1.3 million cases per year, and can cause skin ulcers and even affect areas such as the oral mucosa and respiratory tract. Brazil is the country with the highest number of cases for the three forms of the disease: cutaneous; mucosal and visceral leishmaniasis, also known as kala-azar. Depending on the causative protozoan, the disease requires different treatment and prognostic approaches. The detection and identification of Leishmania species from different clinical forms of the disease can provide early and appropriate treatment. However, the tools available for diagnosis and treatment are primitive, with little progress, regardless of advances in other medical sciences. The development of a vaccine that is effective against different forms of leishmaniasis is fundamental and has been recommended by the World Health Organization (WHO) as a possible tool for an effective eradication of the disease.
In the field of vaccination, the development of vaccines has been more attractive against Canine Visceral Leishmaniasis (CVL) than for humans, since the proportion of positive dogs in endemic areas reaches about 10, 20, 30 times more than infected people. The priority for CVL is also due to the market issue, since the veterinary products for small animals has skyrocketed in the last two decades. Several vaccines have been tested, including live or inactivated vaccines, purified Leishmania fractions, recombinant antigens, antigen expression by Leishmania plasmid DNA through recombinant bacteria.
On the other hand, the efficacy of the vaccines in humans is still limited. For example, the first attempt of mass protection with live vaccine was made in the Soviet Union in 1937, and obtained about 80% of immunizing infections. In 1941, a study was carried out, immunizing 200 people, and reinoculation confirmed that a single lesion was sufficient to protect the individual against a future reinfection. This type of vaccination was called leishmanization. During this period, the first studies of the live vaccine were carried out in Israel. Many of the vaccines tested previously use dead parasites. The focus of modern research is the use of recombinant proteins, live attenuated parasites, and DNA vaccines. This idea assumes that a good vaccine against leishmaniasis should be molecularly defined and able to induce immune memory in the absence of persistent living organisms.
The need for better treatments and the absence of prophylactic vaccines for human visceral leishmaniasis place this disease in second place in mortality rates among tropical infectious diseases and affects about 200 thousand people per year. It is estimated that Tegumentary (ATL), Mucosal (ML) and Visceral (VL) Leishmaniasis have a prevalence of 12 million cases worldwide, distributed in four continents (Americas, Europe, Africa and Asia).
CRISP technology vaccine may be available in six years
Dr. Abhay Satoskar recounts that his team, composed of researchers from Ohio State University (OSU), Food and Drug Administration (US-FDA), National Institutes of Health (NIH), McGill University, Nagasaki University and Gennova Biopharmaceuticals, developed two live attenuated vaccines by removing the centrin gene in old world Leishmania major (LmCen-/-) species, as well as Leishmania mexicana (LmexCen-/-) species from the new world, using CRISPR technology. “These vaccines are based on the concept of Leishmanization, used for many years in the Middle East, where Bedouin tribes rubbed scrapings of active lesions on the skin of children, in areas such as the feet to protect them from subsequent infections – a kind of live vaccine, called leishmanization,” he adds.
The attenuated LmCen-/- vaccine is in production by Gennova Biopharmaceutical in India, and Phase I clinical trials are expected to begin in 2023. “We expect LmCen-/- to be largely effective against New and Old World leishmaniasis. However, if the vaccine against Leishmania major is less effective for New World leishmaniasis due to species differences, we also have the vaccine against Leishmania mexicana, which is a backup”, details Dr. Satoskar. The expectation is that the vaccine will be available for prevention between five and six years after completion of the Phase I study.
Asked about the fact that perhaps a recombinant vaccine is not enough to promote long-term immunization and that a live vaccine would be necessary, Dr. Satoskar agrees. According to him, the currently used vaccines that provide the best long-term immunity and have enabled the elimination of diseases such as smallpox and polio are live attenuated vaccines. “Live vaccines allow the persistence of the antigen, which may be necessary for long-term immunity,” he says.
Vaccine already in human trials
At the moment the only vaccine experienced in humans is that of Dr. Paul Kayes team, funded by the Wellcome Trust. Based on adenovirus technology, similar to that used in recent coronavirus vaccines from AZ/Oxford, J&J etc., it is composed of a chimpanzee adenovirus (ChAd63) that expresses a synthetic gene, which encodes two Leishmania antigens, KMP-11 (K) and HASPB (H). “KMP-11 is expressed in all trypanosomatids and is highly conserved. HASPB has relatively well conserved N and C terminals, but contains repeats that vary among Leishmania isolates. Our gene (KH) represents a compound of the repeated isolates found in Leishmania donovani isolates from East Africa and India. Although some species of Leishmania do not express HASPB (e.g., L. braziliensis) the compound of two antigens should provide good representation in most species of Leishmania in most geographical areas, explains Dr. Kaye.
The Phase I study in humans with healthy volunteers was conducted in the UK and showed safety and immunogenicity. “The first target was therapeutic vaccination in patients with post-Kala-azar persistent cutaneous leishmaniasis in Sudan. We completed an open label and the Phase IIa safety and immunogenicity study was published in 2021. A randomized placebo-controlled Phase IIb trial was also conducted, which should be completed later this year, adds Dr. Kaye. To date, no studies of prophylactic vaccination against visceral or cutaneous leishmaniasis have been performed in endemic countries, due to the scale and cost of these studies. According to him, to support investment in such trials, a model of controlled human infection (CHIM) of sandfly-borne cutaneous leishmaniasis was developed, which should provide an efficient and economical means to evaluate the protective efficacy of the vaccine in a small number of volunteers. CHIM should be available for use by any investigator with vaccine candidates who have achieved Phase I clinical development. “CHIMs can facilitate early testing of an evidence-based decision on candidates progress in field studies; most of those working in the field are being open and transparent about their plans and working collaboratively towards a common outcome,” he notes.
Asked about the fact that perhaps a recombinant vaccine is not enough to promote long-term immunization and that a live vaccine would be necessary, Dr. Kaye acknowledges this may be the case, but recalls that human vaccine studies will be required to truly understand the longevity of immune responses induced by them. “Unfortunately, data from adenoviral vaccines similar to those used in the SARS-CoV-2 pandemic are complex to interpret due to the rapid spread of the virus and the emergence of variants,” he adds. Still according to him, it is likely to have a balance further ahead. For a fact, there is proven memory longevity associated with single live infection, although how long memory persists in humans using single dose attenuated vaccine strains is currently unknown. “However, live vaccines can face challenges associated with logistics in endemic environments in the country, for example, the cold chain. On the other hand, a non-living vaccine may require reinforcement, but it could benefit considerably from the ease of delivery through existing infrastructure,” he compares.
Dr. Kaye considers himself a strong advocate of the idea that we need to experiment with different platforms and that, given the diversity of leishmaniasis and variation in environments where vaccination can be used (prophylactic vs therapeutic; rural nomad vs urban populations; middle-income countries vs. low-income countries), it may not be a one-size-fits-all case. However, it is unreal to think that we can design a perfect vaccine for all leishmaniasis by working with data from such limited clinical trials. What, unfortunately, is still lacking is a funding platform to sustain and expand clinical trial activity for a realistic period of time to provide results (including in immune memory). The past approach to fragmented short-term financing serves only to extend development deadlines, increase competitiveness, limit the involvement of researchers and ultimately make the prospect of a vaccine more distant than it needs to be, he points out. Finally, dr. Kaye hopes that a vaccine for human leishmaniasis will be made available non-profit.
Brazilian Vaccines
Alexandre Reis, professor of Clinical Parasitology at the School of Pharmacy of the Federal University of Ouro Preto (UFOP), recalls that Brazil was a pioneer in the development, testing and use of vaccines for Leishmaniasis, whether cutaneous and/or visceral leishmaniasis. He mentions that the Father of Leishmaniasis vaccines was Professor Wilson Mayrink (in memoriam) who developed the first vaccine (pentavalent and later monovalent) produced industrially under GMP conditions and tested in several clinical trials for American tegumentary leishmaniasis (ATL). The professor then also used this vaccine in the treatment of ATL associated or not with glucantime (immunotherapy or immunochemotherapy). Later, Professor Odair Gernaro (in memoriam) conducted the first clinical trials in endemic areas with first generation vaccines (ultrasound ruptured antigens) in the endemic area of Montes Claros (MG). At this time, they used homologous antigens (L. infantum) and heterologous of L. braziliensis and L. amazonensis against canine visceral leishmaniasis associated with BCG adjuvant. Soon after, Professor Reis performed several tests with the LBSAp vaccine – Leishmania braziliensis + Saponina as an adjuvant and showed the efficacy of this vaccine.
The first canine VL vaccine was developed by professor at the Federal University of Rio de Janeiro (UFRJ), Clarisa B. Palatnik de Sousa, and her studies culminated in the production of Leishmune, the worlds first immunizing against canine visceral leishmaniasis. Today this vaccine is no longer on the market. Another achievement in the area of vaccines against CVL was obtained by professor and researcher at the Federal University of Minas Gerais (UFMG), Dr. Ana Paula Mora Fernandes, who along with Dr. Ricardo Gazzinelli, developed the second vaccine against CVL, which went to the market under the name Leish-Tec®, points out Professor Reis.
Currently there are other vaccines under study by Brazilian research groups and among them is the one developed by reverse vaccinology (bioinformatics), a polypeptide chimera that has been tested with some adjuvants and demonstrating excellent results in murine models (mice and hamster), vaccines that were developed under the supervision of vaccine development specialist Dr. Reis.










