
Varicella zoster virus Vasculopathy as a Rare Cause of Stroke
VZV can spread centrally from the peripheral nerves, causing neurovascular disorders ranging from ischemic stroke-related large-vessel vasculopathy to arterial dissection and subarachnoid hemorrhage
10/07/2023
Hyperintense areas in bilateral suprathalamic regions in B1000 sequence on diffusion-weighted MRI and Hypointense areas consistent with diffusion-limiting ischemia in bilateral suprathalamic regions on diffusion-weighted MRI ADC sequence
Şimşek F et al. – Varicella zoster virus Vasculopathy
Fatma Şimşek[1], Alper Eren[1] and Nazım Kızıldağ[1]
[1]. Ataturk University, Faculty of Medicine, Department of Neurology, Erzurum, Turkey.
Corresponding author: Fatma Şimşek. e-mail: klamaks@hotmail.com
Authors’ contribution
FŞ: Conception and design of the study, Acquisition of data, Final approval of the version to be submitted, Drafting the article; AE: Conception and design of the study, Final approval of the version to be submitted; NK: Conception and design of the study, Drafting the article.
Conflict of Interest
The authors have no conflict of interest to disclose.
Financial Support
No financial support was used in this study.
Orcid
Fatma Şimşek: https://orcid.org/0000-0003-1662-5534
Alper Eren: https://orcid.org/0000-0002-3717-5272
Nazım Kızıldağ: https://orcid.org/0000-0003-1655-5695
A 72-year-old male patient presented with a decreased level of consciousness. He had no known history of systemic disease. He also had a painful vesicular rash on the scalp three weeks prior that had resolved. His neurological examination, during which he could not respond to verbal stimuli, revealed that his four extremities responded to painful stimuli and that the plantar reflex was downgoing bilaterally. His body temperature was 37.3°C. Diffusion-weighted magnetic resonance imaging (MRI) revealed infarcted areas, indicating diffusion restriction in both suprathalamic regions (Figures 1 and 2). A lumbar puncture was performed. No cells were observed upon direct examination of the cerebrospinal fluid. The microprotein levels were high at 65.4 mg/dL. Polymerase chain reaction (PCR) for varicella zoster virus (VZV) DNA was positive. Serum VZV IgG >1500 mIU/mL was positive, and serum VZV IgM was 2.2 mIU/mL was negative. The patient was given 10 mg/kg acyclovir three times daily for 21 days and 60 mg/kg methylprednisolone for 14 days. The patient began to respond significantly to verbal stimuli in the fourth month of hospitalization. VZV can spread centrally from the peripheral nerves, causing neurovascular disorders ranging from ischemic stroke-related large-vessel vasculopathy to arterial dissection and subarachnoid hemorrhage1. VZV vasculopathy is often chronic and long-lasting. Clinical improvement is possible with antiviral therapy2. Given that VZV is a treatable cause of stroke, its etiology should be investigated even if the rash is not described.
Acknowledgments
None.
References
- Nagel MA, Gilden D. Update on varicella zoster virus vasculopathy. Curr Infect Dis Rep. 2014;16(6):1–8.
- Nagel MA, Cohrs RJ, Mahalingam R, Wellish MC, Forghani B, Schiller A, et al. The varicella zoster virus vasculopathies. Neurology. 2008;70(11):853–60.
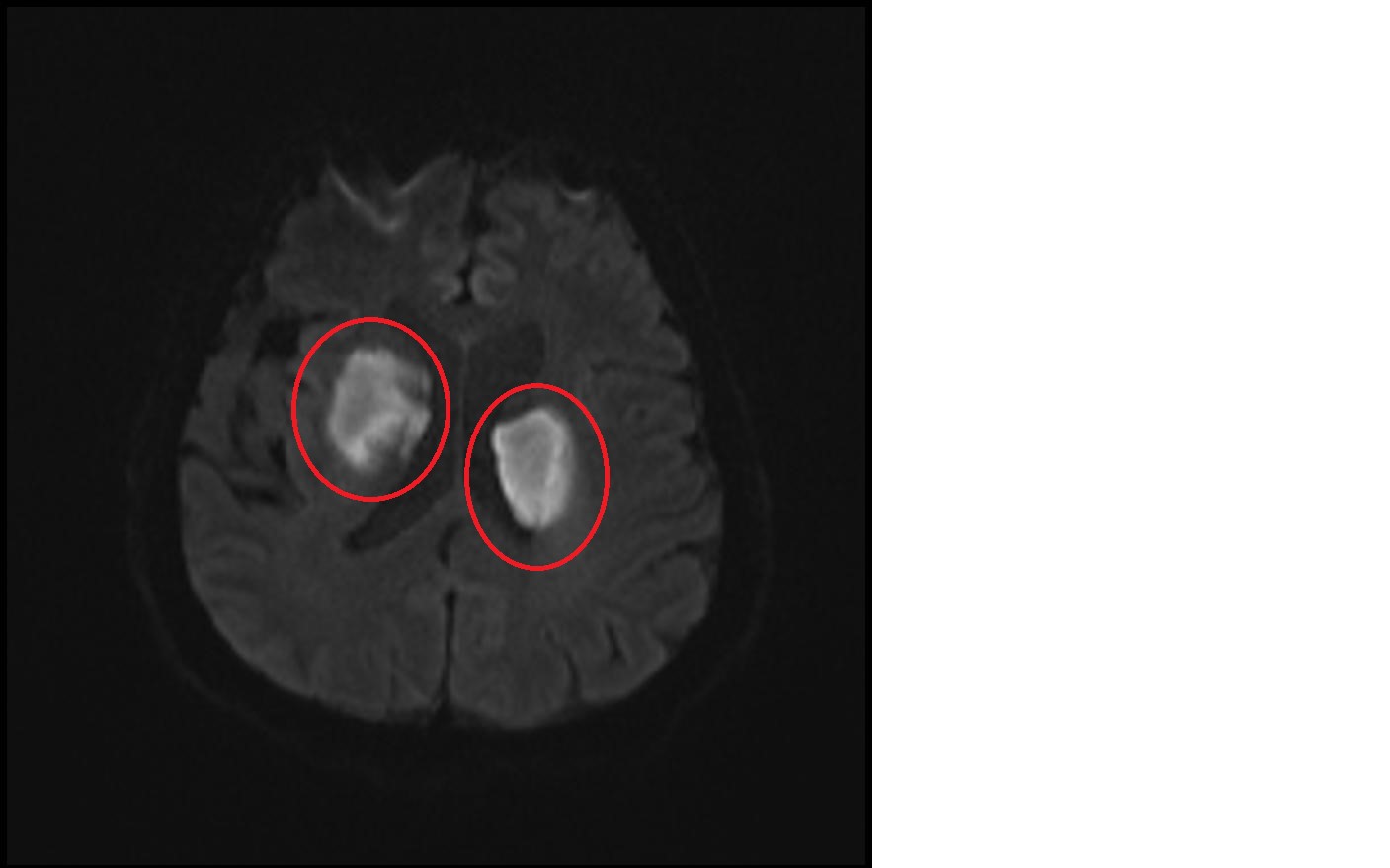
FIGURE 1: Hyperintense areas in bilateral suprathalamic regions in B1000 sequence on diffusion-weighted MRI
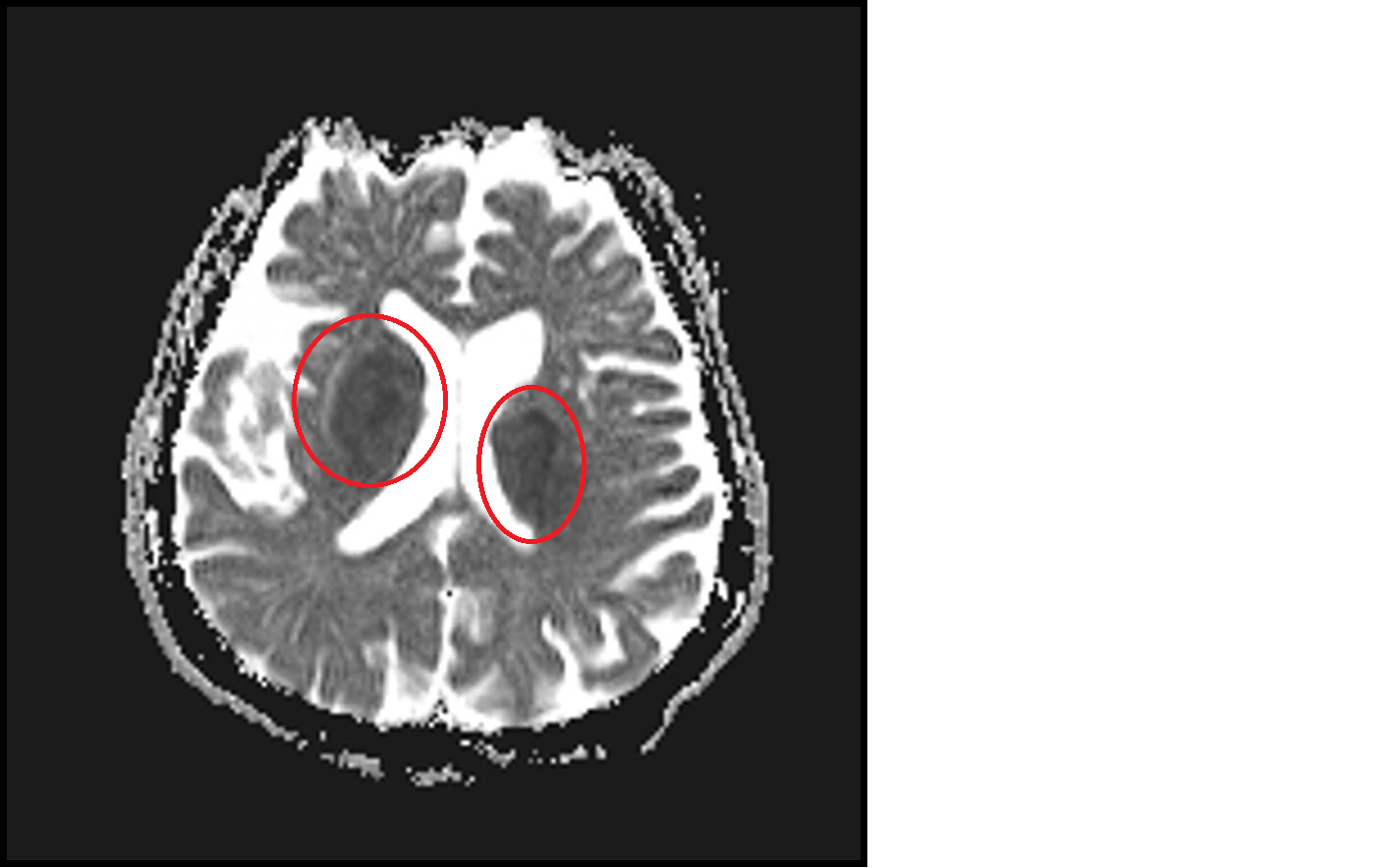
FIGURE 2: Hypointense areas consistent with diffusion-limiting ischemia in bilateral suprathalamic regions on diffusion-weighted MRI ADC sequence










